- Best PCD Pharma Franchise Company
- +91 9216295095
- hcareindia@gmail.com
Teplizumab, New Molecule in Pharma, Can Delay the Onset of Type-1 Diabetes
Cancer Statistics and Data: What We Know and What We Don’t
Data of pharmaceutical sector growth up to 2030
Table of Contents
ToggleTeplizumab: New Molecule in Pharma, Prevention of Type-1 Diabetes
Teplizumab could be a significant development in diabetes treatment, as it could potentially delay the onset of the disease for at least two years for half of the patients.
It is a human monoclonal antibody (mAb) that modifies T cells to prolong the pancreas ability to create insulin. Teplizumab binds with high affinity to the CD3 protein on the surface of certain β cells.
The CD3 antigen is expressed on a specific population of β cells called naive, or pre-β, β cells.
These β cells produce large quantities of immunoglobulins (Ig), which are antibodies that help your body recognize and respond to foreign invaders like microbes, viruses and toxins.
Teplizumab binds with CD3 at its extracellular domain and blocks β cell activation.
This results in decreased production of IgM and IgG antibodies by activated β cells, thus slowing down the process by which type-1 diabetes is triggered and more time for your pancreas to produce insulin.
Teplizumab is an experimental drug that is being developed for the treatment of even stage 2 type-1 diabetes.
This anti-CD3 monoclonal antibody has been shown to slow the onset of type-1 diabetes in mice by delaying the appearance of autoantibodies.
It does so by tethering the immune system to protect beta cells from attack.
Right now, teplizumab is the first drug that can delay the onset of type 1 diabetes that has been approved by the U.S. Food and Drug Administration for human use for this purpose.
In addition, it may also be useful in some other situations as well, such as those involving autoimmune diseases in general and type-2 diabetes in particular.
As we will explore below, let’s take a look at what we know about teplizumab so far and how it may help delay the onset of type-1 diabetes in humans.
Provention Bio received FDA approval for Tzield, new molecule in pharma for Type-1 diabetes.
It is the first-of-its-kind drug that could boost the number of patients who can benefit from it by offering an innovative option for those at risk of type-1 diabetes.
Patients may benefit from months or even years of disease relief because the drug may delay the onset of clinical diabetes.
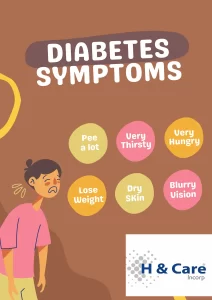
Type-1 diabetes occurs when the immune system attacks and destroys the cells that make insulin.
Person requires insulin injections (or wearing an insulin pump) and must monitor their blood sugar levels constantly in order to survive. Type-1 diabetes can occur at any age, but it is most often recognised in children and young adults.
People with type-1 diabetes are at higher risk if they have a parent, sibling, or son or daughter with the condition, although most patients with type-1 diabetes do not have a family history.
Tzield binds to immune system cells and blocks type-1 diabetes progression to stage 3.
Tzield may slow down the progression of immune system cells that target insulin-producing cells, while boosting the percentage of regulatory T cells. Tzield is given intravenously once daily for 14 consecutive days.
76 patients with stage 2 type 1 diabetes were randomized, double-blind, event-driven, placebo-controlled to assess the safety and efficacy of Tzield.
Once daily via intravenous infusion, patients received Tzield or a placebo. The time from randomisation to development of stage 3 type-1 diabetes was the primary outcome measure.
The trial demonstrated that 43% of the 44 patients who received Tzield were later diagnosed with stage 3 type-1 diabetes, compared to 72% of the 32 patients who received a placebo.
The median follow-up period was 50 months for patients who received Tzield and 25 months for those who received a placebo, resulting in a statistically significant delay in the development of stage 3 type-1 diabetes.
It might cause a range of side effects, including decreased white blood cells, rash and headache, which typically occur in 1 to 3 percent of children treated.
While Tzield is linked to Cytokine Release Syndrome, it may cause hypersensitivity reactions, necessitating the administration of all age-appropriate vaccinations prior to starting it.
It may also interfere with the delivery of all age-appropriate vaccines.
How does Teplizumab work to delay the onset of Type-1 Diabetes?
Type-1 diabetes is triggered by a loss of function of the autoimmune cells in the islet cells of the pancreas. The autoimmune cells are called beta-islet cells. When beta-islet cells are destroyed, the immune system stops producing insulin. Teplizumab binds with CD3 on β cells to reduce levels of IgM antibodies and allow beta-islet cells to increase in number to produce insulin.
β cells produce large quantities of IgM and IgG antibodies. These antibodies are useful in the immune system’s defense against pathogens as well as cancer cells. However, too much of this antibody can be problematic.
Once your β cells produce too many IgM antibodies, they are “turned off” and are no longer able to produce IgG antibodies. This is because the signal that tells your β cells to produce IgG antibodies is supplied by the signal from the IgM antibodies.
Therefore, reducing IgM antibody levels allows your β cells to produce more IgG antibodies, thus slowing down the process by which type-1 diabetes is triggered and more time for your pancreas to produce insulin.
How is Teplizumab used to delay the onset of Type-1 Diabetes?
Teplizumab is given as an intravenous infusion at a dose of 2 mg per 2 mL (1 mg/mL) single-dose vial once daily for 14 days.
Once daily for 14 days, administer TZIELD intravenously for a body surface area-based dose of 65 mcg/m2, 125 mcg/m2, 250 mcg/m2, 500 mcg/m2, and 1,030 mcg/m2 on days 1, 2, 3, 4, and 5, respectively.
Do not give two doses on the same day.
Most patients experience improvement within six months, and many experience improvement within one month.
Since this treatment is highly effective, it is typically reserved for patients with severe type-1 diabetes, those who do not respond to other treatments, or both.
Patients who are candidates for this treatment must be in stable condition and have failed at least one other type of treatment.
How effective is Teplizumab in delaying the onset of Type-1 Diabetes?
Teplizumab is very effective in delaying the onset of type-1 diabetes. The results of a randomized, placebo-controlled trial demonstrated that, compared to placebo, the treatment slowed the rate of progression from type-1 diabetes by a median of 50 months.
However, the participants in this study were selected because they had at least two symptoms of diabetes, including frequent ketosis and inability to produce insulin.
Therefore, it is unknown how well this treatment would work for patients experiencing symptoms of lesser severity.
In Study TN-10, Stage 3 diabetes was diagnosed in 45% of the TZIELD-treated patients and in 72% of the placebo-treated patients.
In order to assess the preventive efficacy of TZIELD, a Cox proportional hazards model was performed stratified by age and baseline oral glucose tolerance test status.
At randomization, the median time from randomization to diagnosis of Stage 3 diabetes was 50 months in the TZIELD group and 25 months in the placebo group, for a difference of 25 months.
After 51 months of follow-up, treatment with TZIELD resulted in a statistically significant delay of Stage 3 diabetes, with a hazard ratio of 0.41.
Does Teplizumab have any adverse effects?
Teplizumab is well tolerated. Common adverse effects include headache, vomiting and rash. Serious side effects are extremely rare, but they include infection at the infusion site, low platelet counts and allergic reaction to the medication.
TZIELD may cause side effects, including Cytokine Release Syndrome (CRS), including: • sickness • tiredness • muscle and joint pain • headache • jaundice.
It may begin with a fever, fatigue muscle and joint ache, nausea, headache, or increased liver enzymes in your blood. Have your healthcare provider right away if you experience CRS symptoms during TZIELD treatment.
TZIELD may cause a decrease in lymphocytes, a type of white blood cell. A decrease in white blood cell count is a serious but common side effect that may damage your body’s ability to combat infections.
After your fifth dose of TZIELD, your white blood cell count will be restored to normal. Some individuals will endure a longer and more severe decrease in lymphocytes.
Can Teplizumab slow down progression of Type-1 Diabetes?
Yes, Teplizumab can slow down progression of Type-1 diabetes by 41%. A meta-analysis of randomised, placebo-controlled studies involving participants did find that the treatment reduced the risk of developing type-1 diabetes by 41%.
This number may seem low, but it is important to consider that type-1 diabetes is one of the best-known autoimmune diseases.